DIGITAL MAMMOGRAPHY WITH 3D TOMOSYNTHESIS

- Mammographic sensitivity for cancer detection varies
- 85.7%–88.8% in entirely fatty
- 62.2%–68.1% in extremely dense
- Digital mammography: Improved sensitivity and accuracy for cancer detection relative to those of film-screen mammography in women with dense breasts (83.6% vs 68.1%, P = .051)
- One of the major limitations of 2D mammography is due to tissue overlap. Overlapping tissue can obscure a lesion causing a false negative result (missed cancer 15-30%). DBT overcomes this limitation by creating 3D images of breast, obtaining multiple 1mm low dose slices of the breast from various angles as the xray tube moves in an arc over the breast. The images are reconstructed using an iterative reconstruction (not isotropic like CT/MRI). For the patient, nothing changes. Positioning, compression, views, time for procedure are pretty much the same. Reduces call back rates. Improves detection & characterization of breast lesions
- After abnormality is seen in mammography, ultrasonography is performed by radiologist on ——– machine. Whole breast US Incremental cancer detection rate above that of mammography was 3-4 per 1000, has limited role for screening. (ACRIN 6666). It is Used for characterization of breast lesion. Cornerstone for diagnostic workup. Used extensively for biopsy guidance. It is modality of choice for palpable masses in young patients. It is Good for differentiating solid & cystic lesions and for For detection of axillary lymphadenopathy. Color Doppler and elastography further help for characterization of lesions.
- Automated Breast Volume Scanner
- Acquires whole series of consecutive B mode pictures & reconstructs 3D data sets of entire breast volume.
- Depicts global breast anatomy & architecture.
- Useful in multifocal lesions
- Good for screening in dense breasts
BREAST ULTRASONOGRAPHY / ULTRASOUND (USG)
Ultrasound is an imaging test by which images of your breast can be viewed on a screen for detecting cancer, by sending high-frequency sound waves through it. It is the poor man’s MRI. At Orchid’s, we use ultrasound in combination with mammography, to increase the sensitivity of the test to nearly 90-95%.
- Ultrasound is the best way to find out the type of an abnormality (whether it is a benign or a malignant tumour, a fluid-filled cyst or solid mass) seen on mammography or felt by physical examination and takes about 5 minutes.
- It helps in better identification of very small breast lesions that are not easily felt by physical examination.
- It is also used for detecting changes in the breast that can be felt but cannot be seen on a mammogram.
- In case of a suspicious lesion, a USG guided needle biopsy is performed, where ultrasound is used to accurately guide the biopsy (tissue removed from the body for examination)

AUTOMATED BREAST VOLUME SCANNER (ABVS)
High-density breasts make it difficult to detect tumour in these breasts using a mammogram, as both the dense tissue and tumour appear white. This is a common occurrence in India and therefore, at Orchids, we use the Automated Breast Volume Scanner (ABVS).
Why this technique?
- ABVS is a standalone system that creates a 3D image of the entire breast, thus providing a comprehensive view of the breast and making tumour detection easy.
- The most important aspect of this system is its automated scanner arm. This automated arm ensures precision, improved patient comfort and reproducibility, as it reduces human errors and does not depend on an operator for the process.
- It can assess and store the breast scans, as well as provide a more understandable representation of the breast’s anatomy and architecture, thus making it efficient in detecting tumour.


MAMMOGRAPHY
After clinical examination by the breast surgeon, patient (>40 yrs) is subjected to mammography in our clinic- Digital mammography with 3D tomosynthesis (machine name). Screening with mammography has resulted in 15-20% reduction in mortality due to breast cancer. Sensitivity of mammography is 68% & specificity is 75%.
- Mammographic sensitivity for cancer detection varies
- 85.7%–88.8% in entirely fatty
- 62.2%–68.1% in extremely dense
- Digital mammography: Improved sensitivity and accuracy for cancer detection relative to those of film-screen mammography in women with dense breasts (83.6% vs 68.1%, P = .051)
- One of the major limitations of 2D mammography is due to tissue overlap. Overlapping tissue can obscure a lesion causing a false negative result (missed cancer 15-30%). DBT overcomes this limitation by creating 3D images of breast, obtaining multiple 1mm low dose slices of the breast from various angles as the xray tube moves in an arc over the breast. The images are reconstructed using an iterative reconstruction (not isotropic like CT/MRI). For the patient, nothing changes. Positioning, compression, views, time for procedure are pretty much the same. Reduces call back rates. Improves detection & characterization of breast lesions
- Automated Breast Volume Scanner
- Acquires whole series of consecutive B mode pictures & reconstructs 3D data sets of entire breast volume.
- Depicts global breast anatomy & architecture.
- Useful in multifocal lesions
- Good for screening in dense breasts
Interventions
- Trucut biopsy- USG guidance
- Vacuum assisted biopsy- for small lesions, papillary lesions, scarless removal of fibroadenomas
- Stereotactic biopsy is performed if the lesion is not seen in USG i.e. microcalcifications.
ELASTOGRAPHY
During breast cancer, the elastic properties of the affected tissues are altered. Elastography is a new technique that detects this change in elasticity and maps it by imaging. It is non-invasive, so the patient need not worry about getting any scars. It is used for characterization of difficult areas. But, doesn’t sonography detect changes in the breast as well? Why should one opt for elastography instead?
Elastography has a major advantage over sonography. Better resolution and clarity result in accurate detections. Whereas, sonography, alone, has the following limitations:
- It cannot distinguish between ultrasound echoes of a normal and a cancerous tissue, that are produced equally.
- It cannot capture areas deep inside the breast, affecting the imaging of dense breasts (as those seen in Indian women).
- It may have trouble distinguishing from other pathologies.
- It cannot show micro-calcifications
- It cannot detect cancers at cellular level.
Benefits of elastography:
- It is reproducible and easily performed.
- It helps to characterize lesions detected on grey scale ultrasound.
- It is useful in planning the management of masses that appear stiff (as they are suspected to be malignant).
- It is used to analyze and differentiate between solid tumours, cysts and other areas of concern during breast ultrasound exams.
BIOPSY
OPEN BIOPSY: OPEN BIOPSY IS UNACCEPTABLE AND IS NOT THE GOLD STANDARD OF TREATMENT
Open biopsy is a surgical procedure, where a cut is made through the skin to expose and remove tissues. It is indicated only when the breast lesion has been studied using mammography or ultrasound, and the lesion has been diagnosed. It is important to note that open biopsy has been made obsolete for diagnosis.
Biopsy (to identify the tumour or illness, when an abnormality is found on imaging) requires inserting a needle inside a lesion on the breast, to remove tissue or cells for examination and analysis. The diagnosis of such suspicious lesions makes it easier to decide the future procedure. As this process only involves a needle, it is painless, scarless, does not change the aesthetics of the breast, and since it is a short OPD procedure, it doesn’t require going to a hospital. This increases the comfort and ease of the person towards this procedure, and the results can be obtained in just two days.
Depending on the lump, the further procedure is decided:
- If the lump is benign (not harmful), no further procedure is required.
- If the benign lump is more than 3 cm, a simple needle excision may be required.
- If the lump is cancerous (malignant), further treatment is planned.
By international standards, minimally invasive biopsy is the most advisable.
Here, at Orchids, we provide four types of biopsies:
- FNAC: It is the simplest method of diagnosing breast cancer but a high inaccuracy makes it unreliable and thus is not recommended. This technique involves insertion of a needle, under local anaesthesia, in the breast lesion to determine its identity (benign or cancerous).
- TRUCUT BIOPSY: Trucut biopsy is the gold standard of diagnosing breast cancer. Trucut biopsy provides several advantages over FNAC, as it has 98% accuracy in detecting breast cancer (benign, pre-malignant and malignant cases), is painless, scarless, and takes 15 mins in the OPD. This type of biopsy uses a thicker needle for removing tiny bits of lesions, which are then identified and can even be saved as further test, if diagnosed as cancerous.
- VACUUM ASSISTED BIOPSY (VAB): The VAB device is a state-of-the-art instrument at Orchids, which provides 99% accuracy in diagnosing even the smallest of lesions (0.2 mm- 0.3 mm size), or even accumulation of (calcifications) calcium salts in the breast, indicating early cancer. It is done within 15 minutes in a day care or an OPD setup, relieving the person from the hassle of going to a hospital. Since it does not involve any surgery, this procedure is virtually painless, scarless, stitchless, and does not distort or damage the aesthetics of the breast either.
- ROBOTIC STEREOTACTIC BIOPSY: There are certain early indicators of cancer such as micro-calcifications, which cannot be diagnosed by physical examination or ultrasound, or even by biopsies using mammogram or sonomammogram. Robotic stereotactic biopsy is the preferred in such cases. This biopsy entails a stereotactic robotic arm which guides the needle in the right place with a 100% precision, thus providing a huge advantage over other biopsies, to diagnose even the smallest of breast lesions accurately, painlessly and scarlessly.
LABORATORY TESTS
Laboratory tests are the mandatory tests to be done before treatment of Breast Cancer. Following are the laboratory tests done at Orchids.
Laboratory tests are meant to identify the tissue removed as benign or cancerous, and to detect the extent to which the cancer has spread. Doctors usually take a decision about which breast cancer treatment is to be given, based on the biopsy report. There are different post-surgery tests, but the laboratory tests in this section are performed before surgery.
There are two types of laboratory tests:
- Histopathological tests: these tests refer to the microscopic examination of the tissue that is removed, in order to study the changes caused by the disease.
- Biochemical tests: these refer to blood and urine tests related to surgery, chemotherapy and overall metabolism.
Following are some of the histopathological tests performed:
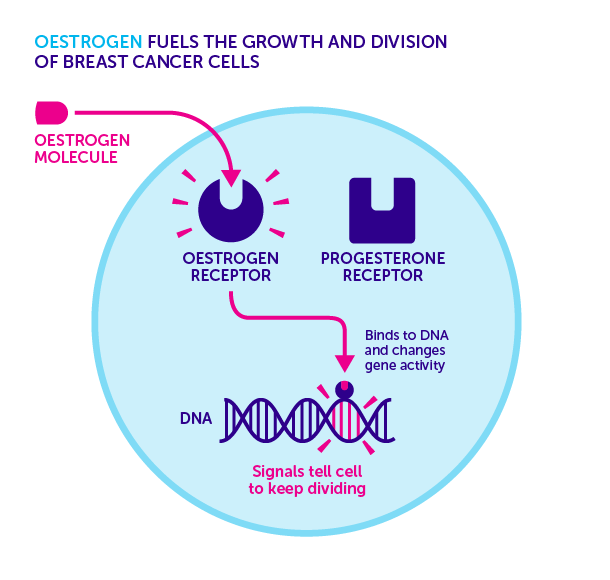
- Hormone receptor status
This laboratory test is an immunohistochemistry-based test. These tests are conducted to determine whether there are hormone receptors present on the surface of the tumour cells.
Oestrogen and progesterone are the two most important hormones governing a woman’s body and health. These two hormones attach to protein receptors present on the cell surface, and accelerate cell growth, in normal as well as some cancerous breast cells. About 2 in 3 breast cancer tumours have receptors for these hormones on their cell surface. Therefore, the biopsy tissue samples should be tested for the same.
If oestrogen receptors are present, then the tumour is referred to as ER positive (ER+) cancer, and if progesterone receptors are present, it is referred to as PR positive (PR+) cancer.
If the tumour cells are positive for the hormone receptors, then hormone therapy is given to the patients.
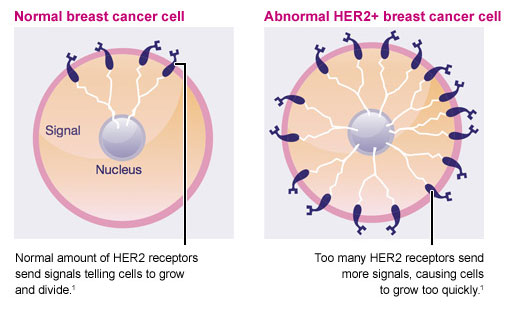
- Human epidermal growth factor receptor 2(HER2)/Neu status:
This receptor has an important function in normal cell growth and differentiation. However, HER2/Neu proteins are sometimes found in breast cancer cells as well. In about 1 in 5 breast cancer cases, the cancer cells have a gene mutation that results in excess production of these proteins. This in turn, promotes the growth of the cancer cells.
HER2 positive tumours are more aggressive and spread faster than ER/PR positive tumours, and are prone to recurrence and poor prognosis. The HER2 gene, that is responsible for production of HER2 proteins, is also associated with ovarian and stomach cancer.
Targeted treatment against HER2/Neu protein can improve the outcome in breast cancer patients who are positive for these protein receptors.
- Ki-67 test:
Ki-67 is a cancer antigen. It is found in growing, dividing cells, but not in cells that with halted growth. This makes it a good marker of breast cancer and can predict the aggressiveness of the cancer, as the cancerous cells rapidly grow and divide. This test measures the level of Ki-67 production in cancer cells.
Based on the Ki-67 levels or score, the doctor can determine the breast cancer prognosis - Fluorescent In-situ Hybridization (FISH):
FISH test maps the genetic changes in cells responsible for affecting the quantity of proteins produced. Changes in production of cell proteins can lead to cancer.
FISH test is advised by the doctor if the breast cancer tumour is diagnosed as HER2/Neu positive. This test is done on the tissue sample obtained by biopsy to see if the cells have extra copies of the HER2 gene. An increased number of copies of the HER2 gene indicates the increase in presence of HER2 receptors. HER2/Neu proteins attach to these receptors and stimulate the growth of breast cancer cells.
This test further helps in deciding which treatment is to be given to the patient. - Genetic tests:
Genetic tests are conducted to diagnose the risk of breast cancer in a woman with a strong family history.
There are two types of genetic tests:
- Germline testing – to detect the presence of BRCA 1- and BRCA 2- associated hereditary breast and ovarian cancer syndrome (HBOC) in the germ cells
- Somatic testing – to identify actionable mutations causing breast cancer, against which targeted chemotherapy can be used. It is usually done when first-line chemotherapy is not responsive.
Germline testing: Germline testing is done for breast cancer risk assessment and risk prediction, and to check the risk to the family members.
BRCA 1 and BRCA 2 genes are the best-known genes linked to breast cancer risk. This test is used for their detection.
BRCA 1 and 2 genes are naturally present in every cell, but some people have a mutation in one or both the genes, thus increasing the risk of suffering from breast cancer, in both men and women. BRCA 1 and 2 mutations can be inherited from either parent.
BRCA 1 carriers have a 60% chance of developing breast cancer by age 70, and an increased risk of developing Triple Negative Breast Cancer (TNBC). TNBC is HER/ER/PR negative cancer, and is worse than ER/PR positive tumours.
BRCA 2 carriers have about 45% chance of developing breast cancer by age 70 and tend to have ER positive tumours.
Germline testing is recommended to determine a person’s BRCA 1 and 2 status, following which, genetic counselling is advised.
Biochemical tests are blood tests and urine tests done for checking the presence of cancer/tumour markers, to detect cancer activity in the body. For example, CA 15-3 test is a biochemical test to detect the presence of CA 15-3 cancer antigen. This antigen is produced by regular breast cells. In many people with breast cancer, there is an increased production of CA 15-3, which enters the blood. Blood tests can then be done to measure the levels of CA 15-3. The higher the CA 15-3 level, the more advanced the cancer. These biochemical tests can thus help in determining further treatment of the patient.
